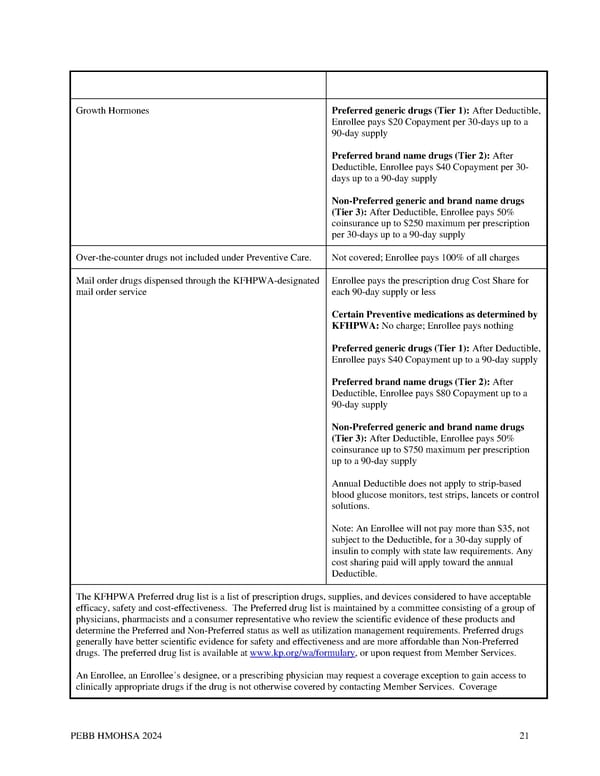
Growth Hormones Preferred generic drugs (Tier 1): After Deductible, Enrollee pays $20 Copayment per 30-days up to a 90-day supply Preferred brand name drugs (Tier 2): After Deductible, Enrollee pays $40 Copayment per 30- days up to a 90-day supply Non-Preferred generic and brand name drugs (Tier 3): After Deductible, Enrollee pays 50% coinsurance up to $250 maximum per prescription per 30-days up to a 90-day supply Over-the-counter drugs not included under Preventive Care. Not covered; Enrollee pays 100% of all charges Mail order drugs dispensed through the KFHPWA-designated Enrollee pays the prescription drug Cost Share for mail order service each 90-day supply or less Certain Preventive medications as determined by KFHPWA: No charge; Enrollee pays nothing Preferred generic drugs (Tier 1): After Deductible, Enrollee pays $40 Copayment up to a 90-day supply Preferred brand name drugs (Tier 2): After Deductible, Enrollee pays $80 Copayment up to a 90-day supply Non-Preferred generic and brand name drugs (Tier 3): After Deductible, Enrollee pays 50% coinsurance up to $750 maximum per prescription up to a 90-day supply Annual Deductible does not apply to strip-based blood glucose monitors, test strips, lancets or control solutions. Note: An Enrollee will not pay more than $35, not subject to the Deductible, for a 30-day supply of insulin to comply with state law requirements. Any cost sharing paid will apply toward the annual Deductible. The KFHPWA Preferred drug list is a list of prescription drugs, supplies, and devices considered to have acceptable efficacy, safety and cost-effectiveness. The Preferred drug list is maintained by a committee consisting of a group of physicians, pharmacists and a consumer representative who review the scientific evidence of these products and determine the Preferred and Non-Preferred status as well as utilization management requirements. Preferred drugs generally have better scientific evidence for safety and effectiveness and are more affordable than Non-Preferred drugs. The preferred drug list is available at www.kp.org/wa/formulary, or upon request from Member Services. An Enrollee, an Enrollee’s designee, or a prescribing physician may request a coverage exception to gain access to clinically appropriate drugs if the drug is not otherwise covered by contacting Member Services. Coverage PEBB HMOHSA 2024 21
 Kaiser Permanente WA CDHP EOC (2024) Page 20 Page 22
Kaiser Permanente WA CDHP EOC (2024) Page 20 Page 22