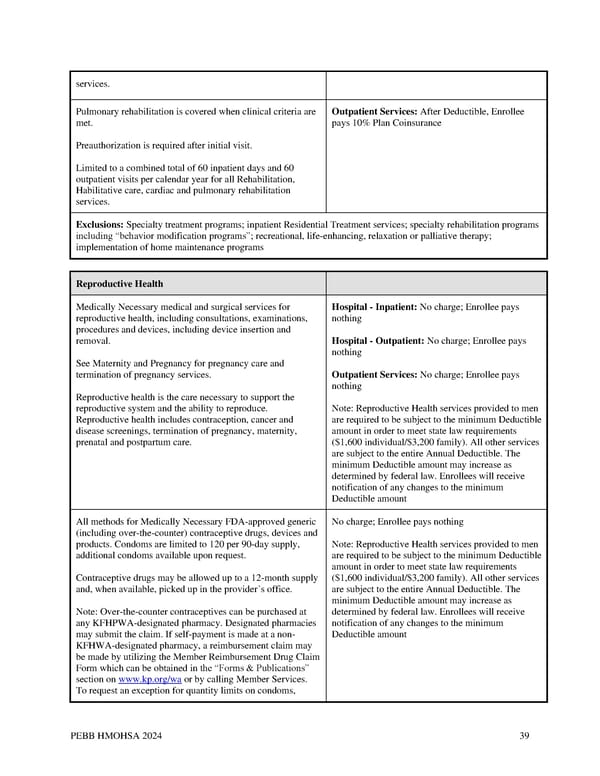
services. Pulmonary rehabilitation is covered when clinical criteria are Outpatient Services: After Deductible, Enrollee met. pays 10% Plan Coinsurance Preauthorization is required after initial visit. Limited to a combined total of 60 inpatient days and 60 outpatient visits per calendar year for all Rehabilitation, Habilitative care, cardiac and pulmonary rehabilitation services. Exclusions: Specialty treatment programs; inpatient Residential Treatment services; specialty rehabilitation programs including “behavior modification programs”; recreational, life-enhancing, relaxation or palliative therapy; implementation of home maintenance programs Reproductive Health Medically Necessary medical and surgical services for Hospital - Inpatient: No charge; Enrollee pays reproductive health, including consultations, examinations, nothing procedures and devices, including device insertion and removal. Hospital - Outpatient: No charge; Enrollee pays nothing See Maternity and Pregnancy for pregnancy care and termination of pregnancy services. Outpatient Services: No charge; Enrollee pays nothing Reproductive health is the care necessary to support the reproductive system and the ability to reproduce. Note: Reproductive Health services provided to men Reproductive health includes contraception, cancer and are required to be subject to the minimum Deductible disease screenings, termination of pregnancy, maternity, amount in order to meet state law requirements prenatal and postpartum care. ($1,600 individual/$3,200 family). All other services are subject to the entire Annual Deductible. The minimum Deductible amount may increase as determined by federal law. Enrollees will receive notification of any changes to the minimum Deductible amount All methods for Medically Necessary FDA-approved generic No charge; Enrollee pays nothing (including over-the-counter) contraceptive drugs, devices and products. Condoms are limited to 120 per 90-day supply, Note: Reproductive Health services provided to men additional condoms available upon request. are required to be subject to the minimum Deductible amount in order to meet state law requirements Contraceptive drugs may be allowed up to a 12-month supply ($1,600 individual/$3,200 family). All other services and, when available, picked up in the provider’s office. are subject to the entire Annual Deductible. The minimum Deductible amount may increase as Note: Over-the-counter contraceptives can be purchased at determined by federal law. Enrollees will receive any KFHPWA-designated pharmacy. Designated pharmacies notification of any changes to the minimum may submit the claim. If self-payment is made at a non- Deductible amount KFHWA-designated pharmacy, a reimbursement claim may be made by utilizing the Member Reimbursement Drug Claim Form which can be obtained in the “Forms & Publications” section on www.kp.org/wa or by calling Member Services. To request an exception for quantity limits on condoms, PEBB HMOHSA 2024 39
 Kaiser Permanente WA CDHP EOC (2024) Page 38 Page 40
Kaiser Permanente WA CDHP EOC (2024) Page 38 Page 40